A Deep Look Into The Use Of Dynamic MRI For Pelvic Organ Prolapse

According to the authors of an abstract presented at the 2022 American Urogynecologic Society/International Urogynecologic Association’s 47th Annual Meeting held virtually and in-person in Austin, Texas from June 14-16, 2022, the use of dynamic MRI for pelvic organ prolapse is essential for pelvic reconstructive surgeons to properly counsel patients and interpret radiographic findings.
Concurrent pelvic organ prolapse and rectal prolapse occur at a rate of approximately 40%. Furthermore, especially with multi-compartmental prolapse, the authors advocate for a multidisciplinary approach in the workup and surgical management of these patients.
Dynamic pelvic MRI has become the main tool for posterior compartment diseases as a result of this comprehensive approach. Furthermore, the authors cite a 2017 joint recommendation from the European Society of Urogenital Radiology and the European Society of Gastrointestinal and Abdominal Radiology that supports the use of dynamic pelvic MRI, as well as a 2021 consensus statement from the Pelvic Floor Disorders Consortium that recommends magnetic resonance defecography to spawn comprehensive guidance for all clinicians caring for patients with pelvic floor disorders.
The goal of this study was to determine the indications and preparations required for dynamic pelvic MRI, as well as to provide the basic knowledge needed for interpreting imaging with a clinical relevance to specific pelvic floor problems.
The study’s findings revealed that there were numerous lines for differentiating pelvic organ prolapse. The writers describe these lines as follows:
“Of all MRI-based reference locations, the pubococcygeal line has the highest inter- and intra-observer reliability.” At rest, it is acquired by drawing a line from the inferior border of the pubic symphysis to the last coccygeal joint in the mid-sagittal plane.”
“The “hiatus” or “H line” shows the antero-posterior breadth of the levator hiatus on a midsagittal picture and is obtained by drawing a line from the inferior border of the pubic symphysis to the posterior wall of the rectum at the level of the anorectal junction.”
“The’muscle’ or ‘M line’ reflects the vertical descent of the levator hiatus and runs perpendicular from the PCL to the most posterior portion of the H line.”
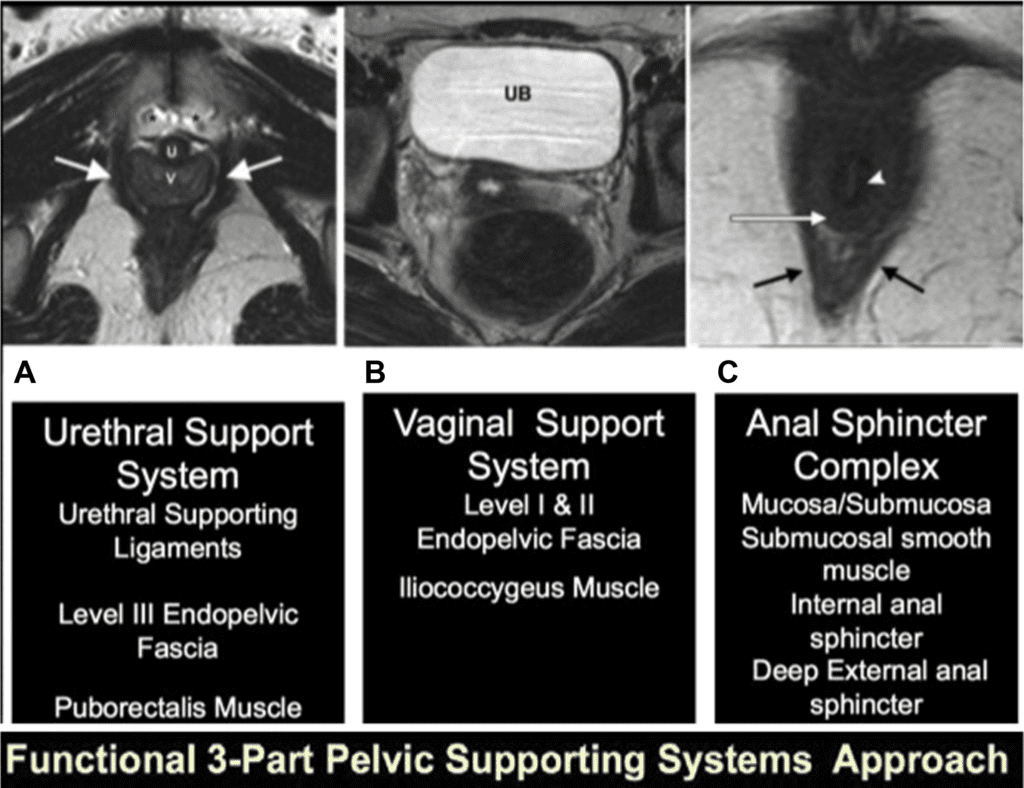
Furthermore, the authors propose that if the rectovaginal fascia is damaged, other tissues such as the small bowel, peritoneum, and sigmoid can herniate through the vagina.
Rectocele and rectal prolapse were also described as posterior compartment disorders. When the rectum prolapses distal to the external anal sphincter and is left untreated for as little as 2 years, the pudendal nerve can be permanently damaged, resulting in faecal incontinence even after surgery. In contrast to rectal prolapse, descending perineal syndrome is defined as an anorectal junction descent more than 2.5 cm from the pubococcygeal line (PCL).
According to the authors, another advantage of dynamic pelvic MRI is the ability to evaluate functional disorders such as paradoxical contraction of the puborectalis muscle. According to the study authors, this occurs when “the rectal angle does not alter or gets more acute and is also related with a lack of pelvic floor descent as well as protracted and incomplete evacuation.”