More Than 1,000 Genes Have Been Identified As Being Associated To Severe COVID-19
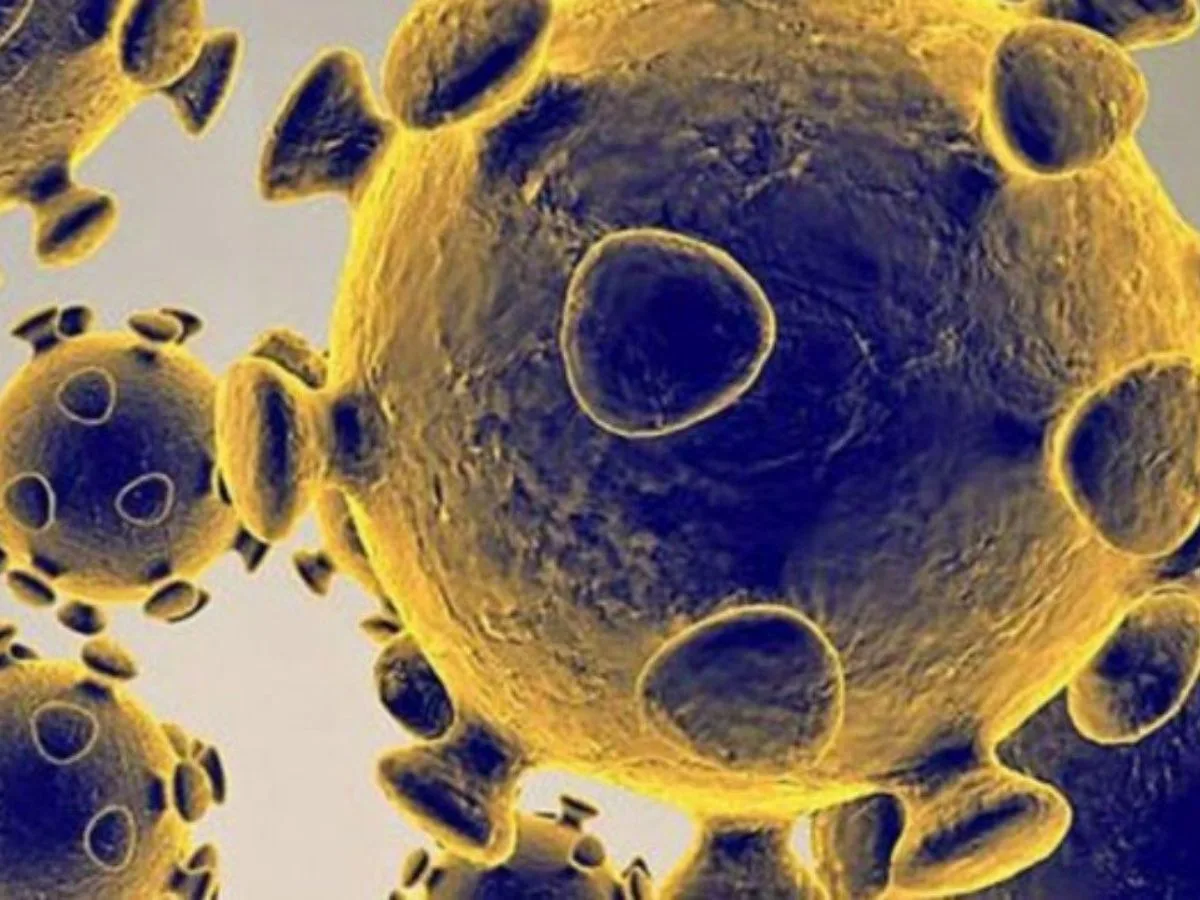
COVID-19, Scientists and medics have tried to understand why some patients infected with coronavirus become very ill or die while others show few, if any, symptoms. Some of the discrepancies are explained by age, BMI, and pre-existing health conditions, but genetics is also thought to have a role.
Researchers from Stanford Medicine and the University of Sheffield in the United Kingdom have discovered over 1,000 genes associated with the development of severe COVID-19 cases that required respiratory support or were fatal. The researchers were also able to pinpoint the types of cells in which those genes were active. It is one of just a few studies that have linked coronavirus-associated genes to specific biological functions.
To assist identify the genetic foundation for complicated and poorly understood disorders, the researchers employed RefMap, a machine learning technology that can find patterns in massive amounts of data.
“We examined the genetic architecture of coronavirus infections and discovered that these 1,000 genes account for 77% of the drivers of severe COVID-19,” Michael Snyder, PhD, professor and chair of genetics, noted.

The research was described in a paper published online on June 14 in Cell Systems. Snyder, the Stanford W. Ascherman, MD, FACS, Professor in Genetics, and Philip Tsao, PhD, professor of medicine, are co-senior authors. Lead authors are genetics teacher Sai Zhang, PhD, and neurologist Jonathan Cooper-Knock, PhD, a Stanford visiting scholar and lecturer at the University of Sheffield.
Looking for solutions
The researchers examined the genetics of severe COVID-19 using two big data sets. The first piece of data included genetic information from healthy human lung tissue. The data assisted in identifying gene expression in 19 various types of lung cells, including epithelial cells, which line the respiratory system and serve as the first line of defence against infection. (Gene expression is the process by which specific genes are activated to produce RNA and proteins.)
The COVID-19 Host Genetics Initiative, one of the largest genome-wide investigations of critically ill coronavirus patients, provided more data. The researchers examined the data for genetic signs — DNA variations known as single nucleotide polymorphisms — that could indicate if someone is at a higher risk of severe COVID-19. They studied if certain mutations were more or less common in COVID-19 patients with severe illness.
NK cells, which are born with you and serve as your body’s first line of defence against infection, are well known for their ability to eliminate viruses and cancer cells. Cooper-Knock said that NK cells contribute to the production of a variety of immune system proteins known as cytokines. Interferon gamma, for example, is a crucial stimulator of immune cells. NK cells, in collaboration with interferon gamma, mount a fast and coordinated response against viral infections.
“CD56bright cells are like the general in command of the battle.” They mobilise other immune cells and instruct them on where to go and what to do. We discovered that key genes in NK cells are expressed less in persons with severe coronavirus infection, resulting in a less strong immune response. Cooper-Knock explained, “The cells aren’t doing what they’re meant to do.”
Snyder compared COVID-19 risk genes to dangerous BRCA gene mutations that predispose some people to breast and ovarian cancer.
“Our findings set the groundwork for a genetic test that can predict who is born with a higher risk of severe COVID-19,” he explained. “Assume there are 1,000 DNA alterations connected to severe COVID-19. If you have 585 of these changes, you may be vulnerable, and you should take all required safeguards.”
Drugs that stimulate sluggish NK cells are already used to treat some types of cancer, according to Cooper-Knock.
“The medications bind to receptors on the NK cells and cause them to respond more strongly,” he explained. NK cell infusion trials for severe COVID-19 are now underway.
The work was also supported by researchers from the University of Sheffield, the Jackson Laboratory for Genomic Medicine, the University of Siena, Azienda Ospedaliero-Universitaria Senese, the University Medical Center Utrecht, the University of Edinburgh, the University of Edinburgh, Western General Hospital, the Royal Infirmary of Edinburgh, and the VA Palo Alto Health Care System.