Pets may play an important role in the survival of methicillin-resistant (MR) and multidrug-resistant (MDR) Staphylococcus spp. in the home. We looked at risk factors for antimicrobial-resistant coagulase-positive staphylococci carriage, with a focus on Staphylococcus aureus and Staphylococcus pseudintermedius isolated from pets in the homes of people with methicillin-resistant S. aureus (MRSA) skin or soft-tissue infection. We analysed cross-sectional data from a 2012 study that assessed the transmission of MRSA and other staphylococci from humans, their pets, and the environment (Pets and Environmental Transmission of Staphylococci [PETS] study).
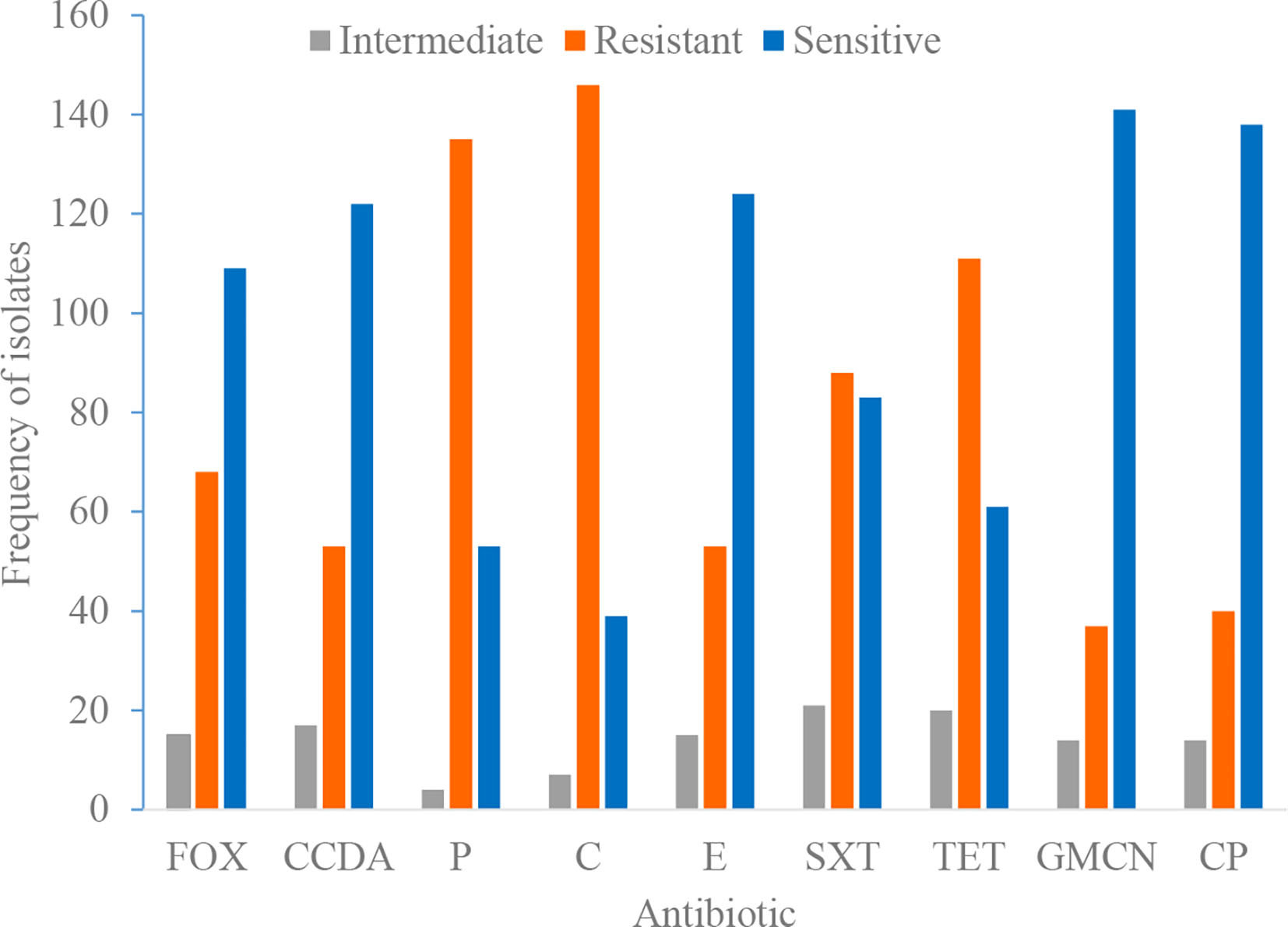
We examined the relationship between demographic, healthcare-related, contact-related, and environmental risk factors and MDR Staphylococcus spp. isolated from dogs and cats using unadjusted and adjusted stratified logistic regression analyses with household-clustered standard errors. These studies included Staphylococcal isolates from dogs (n = 63) and cats (n = 47). The main risk factor of interest was the use of oral or injectable antimicrobials by the pets in the previous year. According to our findings, 50% (12/24) of S. aureus, 3.3 percent (1/30) of S. pseudintermedius, and 25% (14/56) of other coagulase-positive staphylococci (CPS) were MDR. S. aureus isolates were more likely to be MDR than S. pseudintermedius isolates. We found no statistically significant link between the use of oral or injectable antimicrobials in the previous year and the presence of MDR bacteria. The findings suggest that the drivers of antimicrobial resistance in household staphylococci may differ by bacterial species, which could have implications for one health intervention strategy for staphylococci as well as inform the investigation of other reverse zoonoses like COVID-19.